Chronic purulent types of otitis
 Otitis media chronica mesotympanalis
Otitis media chronica mesotympanalis
The most characteristic feature of this illness is a prolonged case of discharging from the ear and of hearing impairment. The odorless discharge, which can be mucous or mucous and purulent, causes considerable discomfort to patients suffering from it. This type of otitis can have completely symptom free periods alternating with periods of acute recrudescence of symptoms.
Discharge in the acute phase is white and creamy, possibly purulent, while in the time following the acute symptoms it is mucous, but odorless at all times.
An audiological examination can identify conductive or mixed hearing impairment. Patients are often confused by a lack of pain and a state of general well-being, which makes it difficult for them to realize that they are suffering from a serious illness.
 The illness does not have a single cause but, instead, can be regarded as an end stage of various pathological processes.
The illness does not have a single cause but, instead, can be regarded as an end stage of various pathological processes.
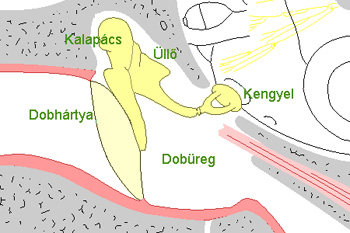
Inflammation is largely limited to the mucous membrane, although in rare cases the bony parts of the middle ear – the auditory ossicles and the mastoid bones, e.g. the longer part of the incus – are also damaged.
Unlike under cholesteatoma, these processes of bone deterioration are relatively rare. Due to the grave scarry disfigurations of the tissue under the mucous membrane, blood vessels can be blocked, causing a secondary metabolic disturbance in the surrounding bone tissue.
Various factors can affect the development of the process, such as the decreased functioning of the tissue of the mucous membrane, different kinds of pathogens of varying sensitivity, the anatomical characteristics of the middle ear, the aeration state of the osseous system, the quality of the functioning of the Eustachian tube, septal deviation, and chronic maxillary sinusitis.
An important factor is the patient’s state of general well-being, including allergies, immune deficiency, pathologic thinnes, diabetes, etc.
 A successful diagnosis can be aided by details of the history revealing recurring ear dischanging and hearing impairment.
A successful diagnosis can be aided by details of the history revealing recurring ear dischanging and hearing impairment.
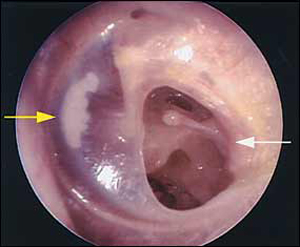
The microscopic image of the ear is very characteristic: a small hole is visible in the middle of the eardrum, often surrounded by small scars.
In case of an acute discharge, small polips also often appear due to the swelling and thickening of the mucous membrane.Discharge is mucous or mucous and purulent, but always odorless.
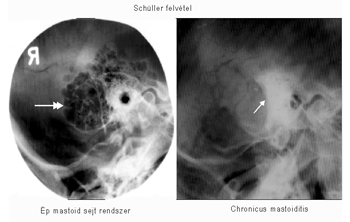
X-rays (or Schüller’s X-ray pictures) show a blocking of the aeration of the mastoid process.
An audiological examination can identify conductive or mixed hearing impairment.
 The illness has to be differentiated from cholesteatoma, which involves a small hole at the edge of the eardrum and stenchy rather than odorless discharge.
The illness has to be differentiated from cholesteatoma, which involves a small hole at the edge of the eardrum and stenchy rather than odorless discharge.
Similar changes characterize the middle-ear infection that develops due to tuberculosis, but that involves multiple perforations of the central region of the eardrum and hearing impairment is severe.
In case of a malignant tumor of the middle ear, eardrum perforation occurs at the edge of the ear drum, in which case extensive growth of tissue extends to the auditory canal and bone destruction at the wall of the auditory canal also occurs.
 In the case of discharging from the ear, the first step is conservative treatment with the aim of “drying up” the middle ear.
In the case of discharging from the ear, the first step is conservative treatment with the aim of “drying up” the middle ear.
The auditory canal has to be cleaned periodically and the discharge drained from the tympanic cavity. In the acute phase the discharge should be submitted to bacteriological examination, and, based on the antibiogram, aimed systemic and local treatment should be applied. Some antibiotics may damage the inner ear, which needs to be taken into account when assigning treatment.
 In the chronic phase, which involves moderate ear discharging and a swelling of the mucous membrane, treatment with 3% alcohol-resorcinol solution and 1‰ potassium permanganate solution is recommended. Boric acid powder or ear drops with boric alcohol are also effective. Polips should be removed from the tympanic cavity, and any inflammations in the nasopharynx and the accessory sinuses should also be treated.
In the chronic phase, which involves moderate ear discharging and a swelling of the mucous membrane, treatment with 3% alcohol-resorcinol solution and 1‰ potassium permanganate solution is recommended. Boric acid powder or ear drops with boric alcohol are also effective. Polips should be removed from the tympanic cavity, and any inflammations in the nasopharynx and the accessory sinuses should also be treated.
After the ear is dried up, surgical treatment should aim to remove inflammatory foci in the temporal bone and the tympanic cavity and to reconstruct the damaged auditory conduction system, the eardrum, and the auditory ossicles.
 These surgical procedures are commonly referred to as typanoplasty. Untreated patients will experience a periodic recurrence of the disease.
These surgical procedures are commonly referred to as typanoplasty. Untreated patients will experience a periodic recurrence of the disease.
Repeated superinflection is caused either by external factors (e.g. bath water) or illnesses of the upper respiratory system extending from the nasopharynx to the ear.
Hearing impairment may gradually increase. Tympanoplasty should be performed as soon after preparation as possible, since malformations of the auditory conduction system will get gradually worse due to recurring inflammations.
If hearing impairment reaches the point where a hearing aid is necessary, tympanoplasty should nevertheless be performed since otherwise continuing discharge from the ear will make it impossible for the patient to wear the hearing aid.
Otitis media chronica cholesteatomatosa

This type of otitis is characterized by a stenchy discharging from the ear, gradually declining hearing, and ear ache and fever during acute flare-ups of the disease.
A dull headache or feeling of pressure in the head may also occur. Discharging from the ear is sometimes very minor or even absent, but when present it is never transparent and mucous as in the case of chronic mesotympanal otitis.
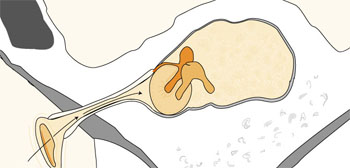
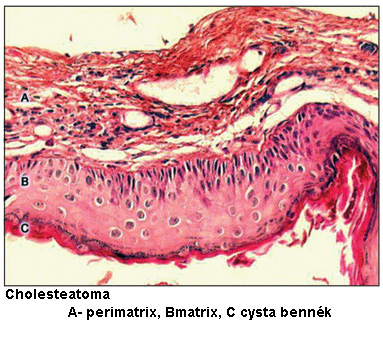 The central feature of the disease is that the peeling epithelial cells of the keratinized pavement epithelium collect and form keratin pearls or cholesteatomas, which can trigger pathological processes when collected in greater numbers in places between tissues or in body cavities.
The central feature of the disease is that the peeling epithelial cells of the keratinized pavement epithelium collect and form keratin pearls or cholesteatomas, which can trigger pathological processes when collected in greater numbers in places between tissues or in body cavities.
In such places the epithelium forms a cyst, and the matrix (i.e. the keratinizing basal layer) is positioned towards the inside of the cyst. The keratin deposits in the cyst like onion layers.
There are different reasons why keratin pearls or cholesteatomas can develop in the middle ear.
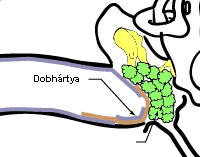
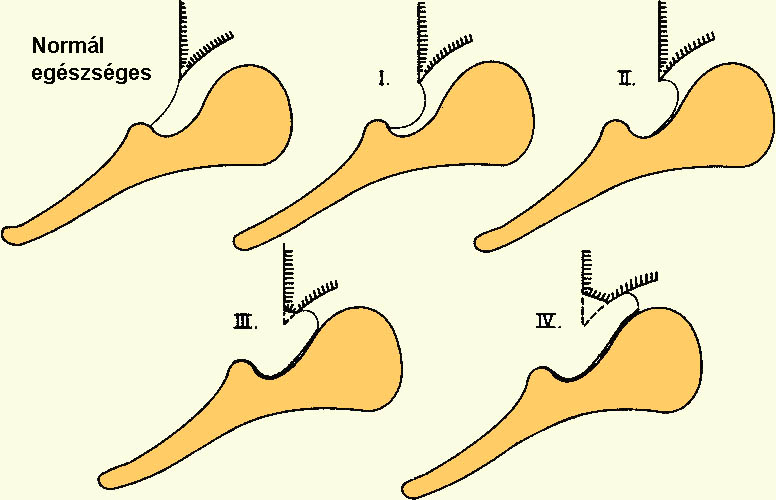 1. Due to a damage in the functioning of the Eustachian tube, negative pressure develops and persists in the middle ear, with the eardrum being sucked in towards the tympanic cavity as a result, which destroys its fibrous system and parts of the eardrum atrophy.
1. Due to a damage in the functioning of the Eustachian tube, negative pressure develops and persists in the middle ear, with the eardrum being sucked in towards the tympanic cavity as a result, which destroys its fibrous system and parts of the eardrum atrophy.
Least resistant parts – such as its postero-superior quadrant or the Shrapnel’s membrane – develop a small keratin sac, which deepens and develops further into a cholesteatoma if the keratinized cells can no longer empty from it. This is the most frequent way in which a cholesteatoma develops.
2. Congenital cholesteatoma: epithelial cells “lose their way” during their development. Such cholesteatomas usually develop on the inside of the utricle, the center of balance, and only more rarely in the cavity system of the middle ear.
 3. Rarely it happens that keratinized cells get into the tympanic cavity as a result of puncture, the fracture of the petrous bone, or other damage to the eardrum (e.g. traumatic rupturing of the eardrum, the insertion of a tympanostomy tube, or tympanoplasty).
3. Rarely it happens that keratinized cells get into the tympanic cavity as a result of puncture, the fracture of the petrous bone, or other damage to the eardrum (e.g. traumatic rupturing of the eardrum, the insertion of a tympanostomy tube, or tympanoplasty).
4. Even more rarely, non-keratinized pavement epithelium lining the inside of the cavity system keratinizes and forms a cholesteatoma.
A cholesteatoma applies constant pressure to its environment, causing the bony substance to slowly erode, forms closed to the outside to open up in time, and, sooner or later, the cholesteatoma gets infected.
The deposited keratin starts to decompose and, because pathogens are various and anaerobic putrifying bacteria are very frequent, the discharge is stenchy.
The products of inflammation, bacterial enzymes and enzymes developing in epithelial tumors (such as collenase) and bony structures eroding under the pressure of the cholesteatoma are constantly decomposing, and the cholesteatoma extends the purulence process to the destroyed areas (increasing the danger of complications).
 This process of destruction causes the auditory ossicles to erode as well, causing a dramatic impairment of hearing.
This process of destruction causes the auditory ossicles to erode as well, causing a dramatic impairment of hearing.
The formation of a cholesteatoma and the process of destruction can be further aided by the factors discussed under chronic mesotympanal otitis.
Cholesteatomas can be categorized by the positioning of the epithelial tumor:
o Pars tensa type cholesteatoma
o Flaccid part type cholesteatoma
o Occult type cholesteatoma
Pars tensa type cholesteatoma: It develops from a sac in the postero-superior quadrant of the pars tensa. The orifice of the sac appears clinically as a perforation at the postero-superior edge.
Perforation at the subtotal edge is rare. Inflamed granulation tissue called “guard polyp” often develops at the edge of the perforation. This is accompanied by strong odor, the discharge contains cholesteatoma laminae, and the surrounding bones (the postero-superior portion of the wall of the auditory canal) erode.
As a result of the auditory ossicles (most often in the joint connecting the incus and the stapes), conductive hearing loss results.
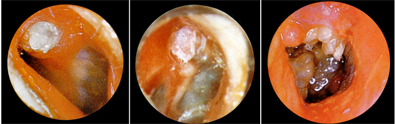
Flaccid part type cholesteatoma: Microscopic analysis can detect a Shrapnell perforation, often covered by crust, removal of which often discloses the erosion of the outer wall of the tympanic cavity. In the tympanic cavity inflamed granulation tissue and cholesteatoma laminae are found and strongly odorous discharge is detected. Conductive hearing impairment occurs, and the inner ear is also damaged in more dvanced cases.
Occult type cholesteatoma: It develops slowly and has no symptoms for a longer time. The eardrum is intact. The air content of the mastoid process and the folds of the mucous membrane determine the direction in which the cholesteatoma develops. The occult type cholesteatoma can be congenital or acquired through trauma.
Common diagnostic signals
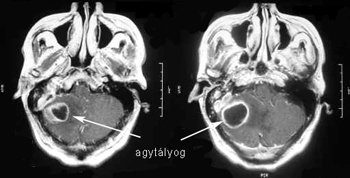
 An important characteristic of the disease is that in Schüller X-rays the air content of bones is inhibited, and the orifice of the mastoid process is rarefied – this cavity is called the cholesteatoma cavity.
An important characteristic of the disease is that in Schüller X-rays the air content of bones is inhibited, and the orifice of the mastoid process is rarefied – this cavity is called the cholesteatoma cavity.
The calcification of the osseous walls of the main veins inside the skull (the sinus sigmoideus) (i.e. the spread of the cholesteatoma into the sinus sigmoideus and transverses as well as into the skull base) as well as the erosion of the bone structure surrounding the central skull base can occur
Stenvers X-rays can show the spread of the cholesteatoma into the organ of balance or the inner ear.
Auditory examination may detect conductive hearing impairment or inner ear damage (mixed type of hearing impairment). If the process spreads into the inner auditory canal, declining neural hearing impairment occurs, resulting in complete deafness (neuritis statoacoustica) accompanied by paralysis of the facial nerve.
During the examination of the organ of balance, as long as its bony wall is intact, spontaneous and stimulated symptoms are absent. In case of the damage of the lateral semi-circular canal, change in pressure elicits a revolving kind of dizziness.
Facial nerves can also be damaged in case of the erosion of the bony facial nerve canal or of spreading into the inner auditory canal.
During diagnosis, the disease needs to be differentiated from inactive chronic mesotympanal otitis (purulent mucous membrane), scarry accretion of the eardrum, auditory canal cancer, and middle ear tuberculosis.
During treatment, due to the nature of the process, conservative methods are not successful, and the treatment of the cholesteatoma is possible only surgically, due to the danger of complications.
 A modern form of surgical treatment is tympanoplasty, whose aim is the assanation of the disease and the subsequent restoration of the hearing function.
A modern form of surgical treatment is tympanoplasty, whose aim is the assanation of the disease and the subsequent restoration of the hearing function.
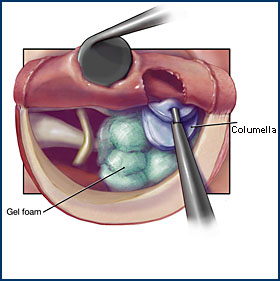
The main aim is the full removal of the cholesteatoma together with the matrix and the perimatrix, and the subsequent restoration of the auditory chain between the eardrum and auditory ossicles.
This involves the closing of the eardrum perforation (from the fascia of the temporal muscle or the perichondrium of the auditory canal), as well as the restoration of direct communication between the eardrum and the stapes base.
Auditory ossicles can be replaced by “short” and “long” ossicles, bone columella, cartilage columella, or plastic prosthesis.
Today tympanoplasty (in case of cholesteatoma) is usually performed in two sittings. In the first sitting the removal of the cholesteatoma, the assanation, and the closing of the tympanic cavity are performed. In the second sitting (usually half a year after the first), the tympanic cavity is examined and the chain of the auditory ossicles is restored.
In certain cases (due to the positioning and extent of the cholesteatoma, complications, or social factors), open tympanoplasty, conservative radical surgery, or classic radical surgery can also be performed.
In the case of these surgical procedured the most important goal is the safe removal of the disease, with no subsequent restoration of hearing.
Cholesteatoma is a very dangerous form of otitis, which can cause serious, life-endangering complications affecting the skull at any time and without symptoms signaling the danger. Its immediate surgical treatment is vital.





