Reflux
The reflux disease

The reflux disease is the most common illness of the digestive system, the symptoms of which affect over half of the population.
The clinical picture was first described by Dr. A. Winkelstein in 1935, who connected the esophageal mucosal deformation with the damaging effect of acidic stomach discharge. The name reflux oesophagitis was first used by dr. Allison, who realized in 1946 that the reflux mechanism plays a crucial role in the development of esophageal mucosal sore.
Many people think that heartburn is a normal accompaniment to eating. Even though it is often experienced after meals or between meals, its cause is not eating per se.
 Medical literature sometimes calls the reflux disease "masked strangler” since it is often hidden behind the symptoms of other diseases.
Medical literature sometimes calls the reflux disease "masked strangler” since it is often hidden behind the symptoms of other diseases.
The disease is hardly known, and sometimes even patients treated for it are not clear on the possibilities of their treatment and cure.
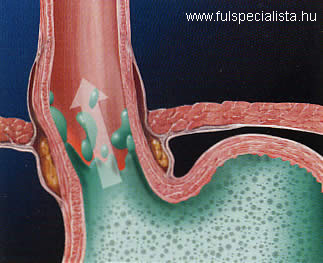
Reflux can occur with healthy people, under natural circumstances, and at this stage it does not cause any symptoms. In such cases the factors protecting and harming the esophagus mucosa are still in a balance. If this balance is upset and the process becomes permanent, the symptoms of the reflux disease develop.
 The sum of the complaints and symptoms associated with and complications from reflux are called the reflux disease. After the full name of the disease, Gastro-Esophageal Reflux Disease, it is also sometimes referred to as GERD in the medical literature.
The sum of the complaints and symptoms associated with and complications from reflux are called the reflux disease. After the full name of the disease, Gastro-Esophageal Reflux Disease, it is also sometimes referred to as GERD in the medical literature.
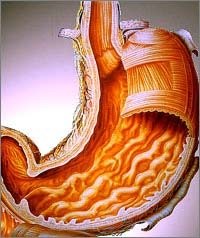
GERD is a complex malfunctioning of the upper section of the digestive canal. As a result, the stomach and duodenal contents mixed with stomach acids and digestive juices reverse their direction and come back up into the esophagus, causing unpleasant symptoms and, as a final stage, organic changes and mucositis.
Its most characteristic symptom is regular and frequent heartburn caused by the fluids from the stomach, and burning pain and a choking feeling behind the sternum.
 Frequency
Frequency
About 80% of the cases of the reflux disease are symptom free, that is, are cases of asymptomatic reflux disease, where direct signs of the disease cannot be detected.
It is well known that most babies “burp” after meals – this is also a reflux of sorts. About 90% of infants grow out of it though.
The frequency of the occurrence of the disease increases sharply in the population over 40 years of age. About 55% of adults suffer from various forms of the reflux disease. About 28% of the population are at increased risk for it.

Milder cases of the disease are more common and make up 60% of all cases.
Interestingly, despite the fact that acidic stomach contents reverse due to abnormal reflux, epithelial injuries (erosions and ulcers) occur only in 30-40% of the cases, which then provide complications affecting the esophagus that occur in 5-20% of all cases.
Up to 7% of the total population experience heartburn every day. More than 48% of pregnant women experience symptoms indicative of reflux.
Symptoms and signs
 GERD often remains hidden behind the symptoms of another disease (asymptomatic reflux).
GERD often remains hidden behind the symptoms of another disease (asymptomatic reflux).
The most common symptom of GERD is heartburn, which affects 83% of all GERD patients.
Acidic stomach contents may spill back into the pharynx and the oral cavity as regurgitation, which might cause chest pain, difficulty in and pain while swallowing.
Atypical, non-alimentary symptoms include cough in 47%, bronchitis in 35%, asthma in 16%, and chronic coarseness in 10% of the cases.
The syndrome is based on abnormal reflux of the upper part of the digestive system, so it is not surprising that in about 20-25% of the cases it can be accompanied by digestive or dyspeptic complaints such as nausea, a feeling of repletion, and distention.
 Since stomach acid is produced only in the stomach, the wall of the pharynx is not prepared to neutralize the strongly acidic effect of stomach acid, which then causes burning pain.
Since stomach acid is produced only in the stomach, the wall of the pharynx is not prepared to neutralize the strongly acidic effect of stomach acid, which then causes burning pain.
Heartburn, then, is a painful, burning feeling originating in the esophagus, which is usually caused by an incompetence of the cardia, the junction orifice of the stomach and the esophagus.
GERD can cause chest pain, which can be similar to the symptoms of coronary heart disease. The symptoms of the latter include a pressing or burning pain at the sternum, radiating to the back, chin, arms or neck.
 Another typical symptom is that small amounts of stomach contents flow back into the mouth.
Another typical symptom is that small amounts of stomach contents flow back into the mouth.
Nighttime heartburn negatively affects the nighttime rest of about 80% of all heartburn patients.
Besides damaging the esophagus, another danger of nighttime acidic reflux is that acidic fluids may flow into the trachea and then the lungs.
In the lungs they can cause recurrent pneumonia or chronic bronchitis. Respiratory symptoms include asthma, chronic cough, chronic pharyngitis, maxillary sinusitis, pneumonia, and laryngitis, as well as hoarseness.
Ear-nose-throat diseases and reflux
 Acidic reflux can cause various ear, nose and throat diseases such as chronic cough, recurring hiccoughs, sore throat, and laryngitis with hoarseness, which can be accompanied by frequent clearing of the throat and a thickening of the vocal chords.
Acidic reflux can cause various ear, nose and throat diseases such as chronic cough, recurring hiccoughs, sore throat, and laryngitis with hoarseness, which can be accompanied by frequent clearing of the throat and a thickening of the vocal chords.
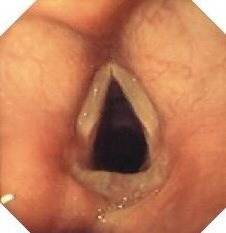 The latter symptoms are due to the fact that the pharynx and the larynx are even harder to defend themselves against the acidic back flow from the stomach than the esophagus.
The latter symptoms are due to the fact that the pharynx and the larynx are even harder to defend themselves against the acidic back flow from the stomach than the esophagus.
Patients are often affected by a scratching, squeezing feeling of a lump in the throat. Pain radiating into the ear is another frequent symptom.
The mucosa of the pharynx, larynx and the accessory nasal sinuses is basically alkaline. A change in the direction of acidity in them causes the mucus producing glands to swell. The swollen glands produce increased amounts of thick mucus, which can cause very unpleasant chronic symptoms when sticking down. Running discharge can cause coughing, especially in the evening, and frequently recurring catarrh in children.
 Reflux can cause asthmatic symptoms. Several studies have shown that the occurrence of reflux among asthma patients is much higher than in the general population.
Reflux can cause asthmatic symptoms. Several studies have shown that the occurrence of reflux among asthma patients is much higher than in the general population.
In addition, GERD can also cause asthmatic attacks, with the two diseases thus strengthening each other and causing ever aggravating symptoms and problems.
Beyond all this, pathological innervation of the bronchial wall can also explain that the acidic back flow in the esophagus increases the sensitivity of the respiratory tract, which, in turn, can increase the occurrence of asthmatic attacks in asthma patients.
Finally, difficulty swallowing, vomiting, weight loss and bleeding can occur as alarm symptoms, indicating serious complications of the disease.
Course of the disease
 The unique cells of the stomach produce hydrochloric acid from water and the chloride ions of sodium chloride, while the free sodium ions react with carbon dioxide produced during cellular respiration forming sodium bicarbonate, which acts as a buffer.
The unique cells of the stomach produce hydrochloric acid from water and the chloride ions of sodium chloride, while the free sodium ions react with carbon dioxide produced during cellular respiration forming sodium bicarbonate, which acts as a buffer.
The two processes occur in a parallel fashion: the more hydrochloric acid is produced in the stomach, the more bases are produced at the same time.
When the acidic stomach contents are passed into the small intestine, the stongly alkaline digestive fluids of the pancreas and the gall bladder neutralize them, again producing sodium chloride, water and carbon dioxide from the alkali and hydrochloric acid.
 Since the process of neutralization usually requires more alkali than are formed at the same time, the body has to produce alkali reserves, which, in turn, requires a satisfactory intake of alkali foods.
Since the process of neutralization usually requires more alkali than are formed at the same time, the body has to produce alkali reserves, which, in turn, requires a satisfactory intake of alkali foods.
A healthy, full diet is rich in fruits and vegetables of high alkali content (potassium, calcium, sodium, and magnesium), which help avert overacidification.
The organic acids contained in fruit decompose into carbon dioxide and water, while alkali elements remain intact. In the case of increased acidification, alkali supplement intake is necessary.
 Factors causing disposition to the disease
Factors causing disposition to the disease
Factors causing a disposition to reflux include an increased intra-abdominal pressure (obesity, tight clothing, pregnancy), eating before going to bed, coffee and alcohol consumption, smoking, certain medications, and horizontal posture.
The consumption of some foods can also be associated with GERD, such as citrus fruits like oranges and lemons, chocolate, greasy and fried food, menthol, spicy food, food containing tomatoes (e.g. spaghetti sauce, chili, pizza, etc.), tomato juice, coffee, tea, Coke, and carbonated soft drinks.
Diaphragmatic hernia can also contribute to the development of GERD. Diaphragmatic hernia results when the upper part of the stomach protrudes through a defect in the diaphragm. The diaphragm normally helps the muscles closing the lower esophagus keep acids in the stomach. Thus, diaphragmatic hernia can contribute to the development of GERD. It can occur at any age and has been shown to occur with many healthy individuals over the age of 50.
 Complications
Complications
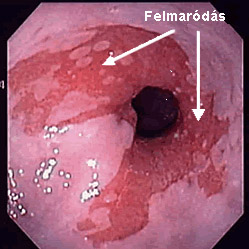
Complications resulting from GERD include esophagitis and esophageal ulcer, which can cause surface mucosa injury or deeper epithelial injuries such as ulcers.
Complications such as the scarring or narrowing of the esophagus usually develop in the lower third of the esophagus in about 10-20% of all cases. Bleeding occurs in less than 5% of all cases of esophagitis.
Unfortunately, states preceding cancer can also develop from GERD.
 Diagnosis
Diagnosis
The most modern diagnostic procedure is endoscopy of the upper part of the digestive tract, which makes direct observation of the esophagus and a histological examination possible.
E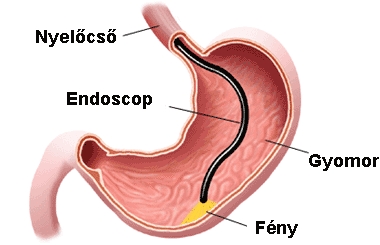
24-hour esophageal pH monitoring is a very effective diagnostic procedure during which a tube is inserted into the esophagus through the nose in order to measure acidity levels in the esophagus.
 Treatment
Treatment
Heartburn patients do not have to put up with the suffering caused by the condition.
Changes of diet and life style, a general deacidification of the body and medications inhibiting acid production ease the symptoms of most patients.
What is the purpose of the treatment?
In the case of mild symptoms the purpose of the treatment is to reach a symptom free state. In the cases of injury or ulcer of the esophagus a further aim is to cure the abnormalities of the mucosa and to prevent complications.
Avoiding foods and medications that prevent the normal closure of the orbicular muscle of the lower esophagus may be important in the treatment of GERD as well.
Avoid greasy foods, chocolate, alcoholic beverages, spices, coffee, tea and smoking as well.
Avoid medications containing theophillin and nitrate as well as some hypotension medications.
 Some antiphlogistic medications damage the walls of the esophagus and prolong recovery. Weight loss as well as elevating the head of the bed by about 15 centimeters (about 6 inches) can be effective. Avoiding eating late at night can also alleviate symptoms.
Some antiphlogistic medications damage the walls of the esophagus and prolong recovery. Weight loss as well as elevating the head of the bed by about 15 centimeters (about 6 inches) can be effective. Avoiding eating late at night can also alleviate symptoms.
Diet
Eating small amounts of food regularly is very important for reflux patients. Avoid strong spices, acidic food, alcoholic beverages and smoking.
Drink freshly squeezed fruit juices (avoid citrus fruits though), a cup of medicinal tea, and eat a few pieces of fruit in the morning. Eat cereals, natural yoghurt, and drink vegetable milk.
Eat warm soups, vegetables and salads for lunch. Meat eaten with raw vegetables is less fattening than traditional side dishes.
 at raw vegetables or fruit as afternoon snack and do not have a heavy meal after 6 PM.
at raw vegetables or fruit as afternoon snack and do not have a heavy meal after 6 PM.
Eating a piece of fruit, a cup of yoghurt or some salad is allowed before going to bed.
Drink 2 liters of filtered water, medicinal tea or non-carbonated mineral water a day.
Avoid carbonated soft drinks with sugar since these increase the level of the body’s acidity.
For many patients diet change is not enough or daily stress is unavoidable. In such cases supplements are recommended.
 We recommend supplementsthat restore alkali reserves from natural substances and bind unnecessary acids.
We recommend supplementsthat restore alkali reserves from natural substances and bind unnecessary acids.
The product primarily recommended by us contains a unique mixture of 49 different organically grown vegetables, grasses, leaves and sprouted grains.
It contains more than 125 natural vitamins, minerals and amino acid, which makes the maximal absorption of alkali possible.
It has an energizing effect and helps the oxygen intake of blood from water. It is a strong oxygen catalyst and helps the optimal functioning of body cells. It alkalinizes the body and reduces overly high acid levels. This alkaline powder is capable of compensating for high acid levels in the blood and bind stomach acids as well.
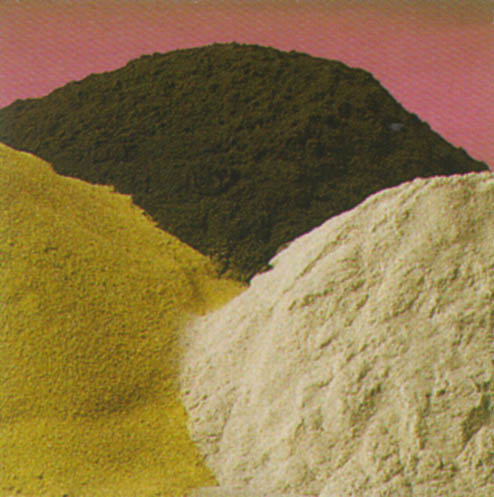 The powder recommended by us has to be taken during the day dissolved in water. This product can successfully reduce acid level, detoxify and energize in a matter of a few weeks.
The powder recommended by us has to be taken during the day dissolved in water. This product can successfully reduce acid level, detoxify and energize in a matter of a few weeks.
For more information,
read the product information or manufacturer’s homepage.
With other questions, call at +36-20-397 4144 or send email to This email address is being protected from spambots. You need JavaScript enabled to view it.
About the product and ordering click here
Drug treatment
The purpose of drug treatment of GERD is to reduce the irritating effect of acidic stomach contents flowing into the esophagus. It is possible through drug therapy accompanying life style changes.
 The most effective medications are those reducing the production of stomach acids.
The most effective medications are those reducing the production of stomach acids.
Certain medications such as antacids as well as medications neutralizing acidity are effective only in mild or medium serious cases of GERD.
Antacids for milder cases can be purchased without a prescription, but their effect is only very temporary.
Proton pump inhibitors are the most effective in reducing gastric acid secretion. The new generation of proton pump exhibitors have a very even effect and alleviate or even cease reflux symptoms already within 24 hours.
Medications reducing the production of stomach acids do not completely block the production of stomach acids, so the acidic environment necessary for the functioning of digestive enzymes is retained.
 In 80% of the cases the disease requires a longterm treatment due to relapses. Treatment is chosen to fit the symptoms. In milder cases (such as 1 or 2 episodes after meals per week) liquid antacids are prescribed.
In 80% of the cases the disease requires a longterm treatment due to relapses. Treatment is chosen to fit the symptoms. In milder cases (such as 1 or 2 episodes after meals per week) liquid antacids are prescribed.
According to modern treatment principles accepted today, medication suppressing the production of stomach acids is recommended for 8-12 weeks, in decreasing amounts, following gastroscopy, which is an examination necessary to rule out complications.
Surgical treatment is also possible, but it is necessitated in cases when prolonged maintenance therapy can be expected, especially in young patients. Surgical therapy can be performed on the recommendation of the specialist, following detailed examination, in specialized medical institutions.
Due to high recurrent rates, maintenance treatment is often necessary, in which proton pump inhibitors have been shown to be most effective. Grave cases that do not respond to medical treatment as well as some complications may require surgical treatment as well.
Hits: 5959