Maxillary sinusitis
Inflammation of sinuses
General characteristics
 Inflammation of the sinuses is a very common disease.
Inflammation of the sinuses is a very common disease.
It is estimated that about 5% of the Central European population suffers from chronic sinusitis.
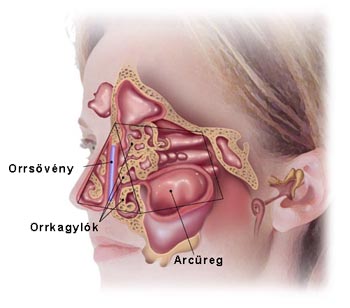
Clinically, in adults the most commonly affected is the maxillary sinus, followed by the ethmoid cells, the frontal sinus, and finally the sphenoidal sinus.
In children the inflammation of ethmoid cells is most common.
If more sinuses are affected, the case is referred to as polysinusitis, if all of them, pansinusitis, unilateral or bilateral.
The most common way of development of the sinusitis is when the inflammation of the nasal cavity spreads to the maxillary sinus. Theoretically, in all cases of rhinitis, the mucous membrane of the maxillary sinus is also affected (in what is called concomitant maxillary sinusitis), however, usually clinical symptoms do not occur.
The inflammation is caused by viruses or bacteria, but very often mixed infection occurs, sometimes accompanied by fungal infection as well. The course of the disease is affected by immunological factors (allergy, anergy), partly by the interaction between pathogens (virulence) and the defense system.
Disturbances in the ventilation of the sinuses can be caused by the acidification of the body. During the detoxification processes, swelling and pathological mucus production occurs in the mucous membrane of the sinuses, since the body tries to free itself from unnecessary acids and poisonous materials produced in the body in binding the acids via nasal discharge as well.
The starting point of sinusitis can be tooth disease (root apex granuloma) as well (10%). This is the disease of the 2nd premolar and 1st molar. The pathogens are usually anaerobes, which makes the discharge of the wound typically odorous. Prerequisite to the successful treatment of the sinusitis is the removal of the diseased tooth.
 The condition commonly known as bath- or pool sinusitis is when acute maxillary sinusitis develops as a result of swimming or diving, as a result of pathogens get into the nasal cavity and/or the accessory cavities from the water. The irritant character of chloride also plays a role in the development of the condition.
The condition commonly known as bath- or pool sinusitis is when acute maxillary sinusitis develops as a result of swimming or diving, as a result of pathogens get into the nasal cavity and/or the accessory cavities from the water. The irritant character of chloride also plays a role in the development of the condition.
Depending on the type and virulence of the pathogen, the general state of the body, and on the type of immunological reaction, first a catarrhal state develops in the maxillary sinus, which then turns into watery or mucous maxillary sinusitis.
If the stagnant discharge is superinfected, the mucous kind of maxillary sinusitis develops. Mixed types of the disease are also common. Pathological changes in the maxillary sinus depend on the length of the period of inflammation: acute (subacute) and chronic types of maxillary sinusitis are differentiated.
 The most typical symptoms are headache and pain in the face, with the latter increasing when the patient bends down, lifts something, coughs etc., that is, when pressure increases in the sinuses. In case of acute maxillary sinusitis pain is much stronger than in the case of the chronic type.
The most typical symptoms are headache and pain in the face, with the latter increasing when the patient bends down, lifts something, coughs etc., that is, when pressure increases in the sinuses. In case of acute maxillary sinusitis pain is much stronger than in the case of the chronic type.
 In case of chronic maxillary sinusitis pain might be completely absent.
In case of chronic maxillary sinusitis pain might be completely absent.
Pain in the accessory sinuses is characterized by a sense of pressure occurring in and/or at the frontal part of the skull as a piercing, drilling or pulsating feeling of pain.
In the case of acute inflammation sensitivity to pressure and percussion is typical in the region above the sinus in question: on the face, above the teeth for the maxillary sinus, on the forehead for frontal sinus, at the corner of the eye closer to the nose for the ethmoid cells, and typically at the nape, the temples or the middle of the head for sphenoidal sinus.
 Nasal discharge:
Nasal discharge:
Unilateral rhinitis, especially in adults, should always raise suspicion of maxillary sinusitis.
Discharge can be colorless and of varying viscosity. The first symptom is blockage of the nose, followed by ample watery nasal discharge.
If the condition develops further, the discharge thickens and turns stringy, and glassy white, due to the increased functioning and proliferation of goblet cells in the mucous membrane.
 If the nasal discharge is infected with bacteria, it ceases to be colorless, turning mucous and yellow, green or bloody. The discharge is often crumbly, mostly odorless, rarely odorous (odor being indicative of inflammation originating in teeth).
If the nasal discharge is infected with bacteria, it ceases to be colorless, turning mucous and yellow, green or bloody. The discharge is often crumbly, mostly odorless, rarely odorous (odor being indicative of inflammation originating in teeth).
Pus may be dripping forward, but also – especially in the case of inflammation of dorsal sinuses – towards the back, to the pharynx, causing coughing. The localization of the flow of the pus and the orifices it originates from helps identify the affected sinus.
A frequent symptom is blocking of breathing through the nose, which can be variable or constant. Unilateral blocking of breathing can be indicative of maxillary sinusitis.
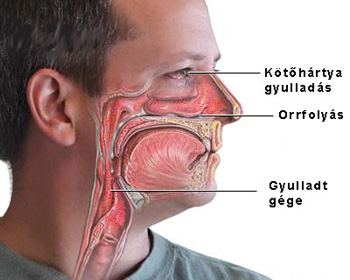
Due to the swelling of the nasal mucous membrane, difficulty in smelling can occur. Maxillary sinusitis originating in dental inflammation can produce strong odor. Nasal discharge can cause eczema at the nostrils, especially in children. Maxillary sinusitis is often accompanied by conjunctivitis.
Coughing, hoarseness and/or bronchitis are indicative of disease in the lower respiratory system.
Of the general symptoms, the most common is exhaustion and apathy. Fever occurs only if the infection is generalized or if complications develop.
Diagnosis: Examination of the nose is necessary for diagnosis. The most common procedures are the direct examination of the nose, nose endoscopy, X-ray, CT scan, ultrasound diagnostics, probing, puncture, lavage of the maxillary sinus, bacteriological examination of the nasal discharge, exploratory exposure and and tissue excision.
Basic principles of drug treatment of maxillary sinusitis:

(a) Acute maxillary sinusitis: nose drops or sprays several times a day to reduce swelling of the mucous membrane by opening the orifices of the accessory sinuses.
Cotton plugs can also be used to get the swelling reducing medicine into the nose.
Use of localized heat (shortwave, infra lights) can also be useful. If the patient feels that the heat is not effective, cold may be applied. At the start of the illness, before the onset of fever, hot packs to induce perspiration or hot baths can be effective. In case of general lack of well-being, bed rest is advised. In case of fever, prescription of antibiotics is recommended only selectively.
(b) Subacute maxillary sinusitis. If no improvement occurs within a week following the administering of the above treatment, puncture and rinsing of the maxillary sinus as well as rinsing with an antibiotic compatible with the antibiogram may be in order. The antibiotic can be administered as an injection if necessary. The above described treatment should also be continued.
(c) Chronic maxillary sinusitis. Rinsing might be effective in treating it. Constant catheterizing (especially for children) can aid treatment. If after 6-10 instances of rinsing no improvement is detected, the sinus needs to be cleaned surgically. In case of an allergic component, the treatment needs to be supplemented with antiallergic treatment.
(d) Since the development of maxillary sinusitis is greatly affected by the acidification of the body, a key component of its treatment is the detoxification and alkalization of the body as well as a careful composition of the patient’s diet. This can be most easily achieved by taking natural alkalizing supplements.
The product recommended by us contains a unique mixture of 49 different organically grown vegetables, grasses, leaves and sprouted grains. It contains more than 125 natural vitamins, minerals and amino acid, which makes the maximal absorption of bases possible. It has an energizing effect and helps the oxygen intake of blood from water. It is a strong oxygen catalyst and helps the optimal functioning of body cells. It alkalinizes the body and reduces acid levels.
The powder recommended by us has to be taken during the day dissolved in water. This product can significantly reduce acid level, detoxify and energize in a matter of a few weeks.
For more information,
read the product information or manufacturer’s homepage.
With other questions, call at +36-20-397 4144 or send email to Ez az e-mail-cím a szpemrobotok elleni védelem alatt áll. Megtekintéséhez engedélyeznie kell a JavaScript használatát.
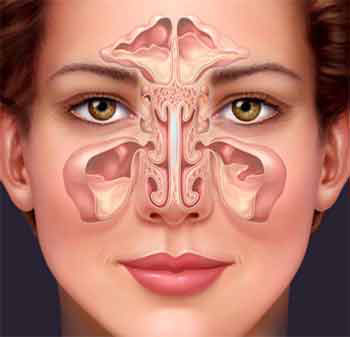
Maxillary sinuses
 Severe pain and a feeling of fullness in the central part of the face usually accompanies bilateral maxillary sinusitis.
Severe pain and a feeling of fullness in the central part of the face usually accompanies bilateral maxillary sinusitis.
Sensitivity to pressure and percussion above the upper canine teeth. The cheeks turn rosy, the nasal conchea swell. Mucous discharge appears in the central nasal passage and at the bottom of the nasal cavity.
In case of chronic maxillary sinusitis pain is usually minor, only a sense of pressure is felt. The affected half of the nose is blocked, mucous or purulent discharge develops (unilateral rhinitis).
The infraorbital nerve radiates pain, the sense of smell is limited, and nasal discharge might be odorous. The nasal conchae and the mucous membrane swell, purulent discharge might occur in the central nasal passage and/or at the base of the nasal cavity, and nasal polyps might develop.
Ethmoid cells
 The symptoms of an acute inflammation of the ethmoid cells are characterized by a lack of pain. Instead, a feeling of pressure and fullness occurs in the area between the eyes and the root of the nose or at the temple.
The symptoms of an acute inflammation of the ethmoid cells are characterized by a lack of pain. Instead, a feeling of pressure and fullness occurs in the area between the eyes and the root of the nose or at the temple.
Breathing through the nose is blocked, and nasal discharge occurs. The sense of smell is limited. The nasal conchae – especially the central area – swell.
Discharge drips from the central and, sometimes, the upper nasal passage.
The symptoms of chronic inflammation of the ethmoid cells:
A diagnosis is often difficult since symptoms are atypical. Chronic (unilateral) rhinitis, tiredness occur, and hysteric globus might occur. Mucous membrane swells in the central nasal passage, polyps may form. Discharge occurs in the central and, sometimes, in the upper nasal passage as well as the dorsal wall of the pharynx. The sense of smell deteriorates or is completely absent. Especially the frontal ethmoid cells may serve as the focus of the infection. CT scan and endoscopy are required for an exact diagnosis.
Frontal sinuses:
An acute inflammation of the frontal sinuses is most often accompanied by severe headache and pain in the forehead. The forehead and the exit point of the supraorbital nerve are sensitive to pressure and percussion. Purulent discharge occurs at the very front of the central nasal passage. The mucous membrane of the central nasal passage is sanguine and often has a glassy swell.
Chronic inflammation of the frontal sinuses is often characterized by only a minor feeling of pressure at the forehead. The exit point of the supraorbital nerve is sensitive to pressure. A limited sense of smell and a pathological sense of smell (cacosmia) can occur. Large frontal sinuses are more susceptible to disease than smaller ones. Polyps often form in the diseased frontal sinus, only rarely haning over into the nasal cavity.
Sphenoidal sinuses:
The symptoms are usually atypical: Pain and a feeling of pressure in the middle of the skull is frequent, radiating to temples or nape. Severe pain in the eyes sometimes occurs. Breathing thought the nose is usually not blocked.
Discharge drips down the dorsal wall of the pharynx or in the upper nasal passage. Merely considering the possibility of the inflammation of the sphenoidal sinuses often takes the physician halfway to the successful diagnosis.
Maxillary sinusitis in children
Symptoms in children are similar to symptoms in adults, however, cases poor in symptoms occur very frequently. The form of the inflammation is most often chronic catarrhal inflammation. Inflammation of the ethmoid cells is possible soon after birth.
Maxillary sinusitis is very rare in infants but is progressively more frequent starting with the age of 4. Inflammation of the frontal and the sphenoidal sinuses typically occurs starting with the age of 5-12. Childhood chronic maxillary sinusitis is most frequent between the ages of 7 and 12 and is often responsible for secondary illnesses (bronchitis and pneumonia, developmental anomalies, low fever of unclear origin, and diseases of the stomach, intestines and kidneys).
Signs for suspicion include irritable coughing, sniffling, prolonged rhinitis, recurrent colds, lack of appetite, developmental anomalies. Diagnosis requires an X-ray of the accessory sinuses and endoscopy.
Special treatment includes a surgical removal of the adenoids and a continuous ventilation and rinsing of the affected sinus. Transnasal surgery might be advised if necessary, however, extensive surgical procedures should be avoided.
The maxillary sinuses and the focus of inflammation
It is estimated that only about 10% of inflammation foci in the head are cases of maxillary sinusitis. Diseases of tonsils and teeth occur as foci of inflammations much more often.
The special characteristics of inflammations in the sinuses
Találatok: 77205




