Surgical correction of hearing
Surgical procedures correcting conductive hearing impairment
The surgical correction of hearing impairment caused by otitis is a great achievement of otolaryngological microsurgery.
The procedures are very widely performed and offer good results in curing the disease and surgical rehabilitation.
Conductive hearing impairment is characterized by good bone conduction, a satisfactory functioning of the auditory nerve, and damage, correctable surgically, in the auditory system, i.e. in the auditory canal, the eardrum, the tympanic cavity, or the auditory ossicles.
Diagnosing conductive hearing impairment is highly important. After precisely defining bone conduction and aeration, surgical procedure can result in the two connecting and hearing being partly restored.
 Recent developments in medicine now also offer correction of various types of conductive hearing impairment, such as the congenital blocking of the auditory canal, the absence of the auditory canal, and congenital developmental anomalies.
Recent developments in medicine now also offer correction of various types of conductive hearing impairment, such as the congenital blocking of the auditory canal, the absence of the auditory canal, and congenital developmental anomalies.
Diagnosing congenital bilateral absence of auditory canal or of pinna is relatively easy.
It is vitally important that hearing impaired infants receive a hearing aid relatively early, possibly at six months of age. Surgical rehabilitation is a relatively complicated procedure, recommended for the experienced otolaryngologist surgeon.
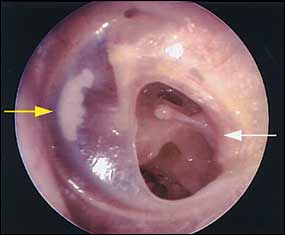
Acquired hearing impairment is much more frequent than congenital conductive hearing impairment: chronic otitis and diseases of the eardrum and auditory ossicles are relatively common.
 In such cases the first step of treatment is the assanation of the chronic discharge production, i.e. the disease is surgically eliminated, followed by a reconstruction and restoration of the auditory system.
In such cases the first step of treatment is the assanation of the chronic discharge production, i.e. the disease is surgically eliminated, followed by a reconstruction and restoration of the auditory system.
The procedure can be performed with the help of surgical microscope in one or two sittings. In case of cholesteatoma, when chronic purulent disrcharge is accompanied by cholesteatoma and on children, it is recommended that the procedure be performed in two sittings.
First the cholesteatoma is operated on in such a way that no radical operation is performed, and, if possible, the eardrum is restored. In a second sitting in half a year’s time the reconstruction of the auditory ossicles is performed.
 The advantage of performing the procedure in two sittings is that at the second sitting it can be checked whether the cholesteatoma relapsed, which is, unfortunately, a rather common occurrence, especially in young patients.
The advantage of performing the procedure in two sittings is that at the second sitting it can be checked whether the cholesteatoma relapsed, which is, unfortunately, a rather common occurrence, especially in young patients.
In the two-phase procedure, however, the relapse can be discovered early, and reconstruction is performed subsequently, bringing better long-term results.
There are two ways for completing the surgical petentration: behind the ear (retroauricularly) or through the auditory canal (endoauricularly).
 The former way of penetration is more taxing for the patient but has the advantage of disclosing the diseased mastoid process as well. Penetration through the auditory canal requires more surgical experience and experience but can be performed in ambulant care.
The former way of penetration is more taxing for the patient but has the advantage of disclosing the diseased mastoid process as well. Penetration through the auditory canal requires more surgical experience and experience but can be performed in ambulant care.
The surgical procedure required in case of dry perforation of the eardrum is much simpler. In such cases reconstruction is performed in one sitting.
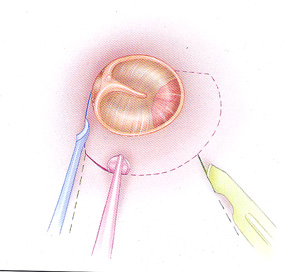
 Replacement of the eardrum, the procedure called myringoplasty, is one of the most common hearing restoration procedures.
Replacement of the eardrum, the procedure called myringoplasty, is one of the most common hearing restoration procedures.
The eardrum can be reconstructed out of connective tissue: the tissue most commonly used for this purpose is fascia from the ear muscle (fascia temporalis).
The advantage it offers is that it is positioned close to the ear, so no special surgery is necessary to remove it, and it also offers tissue of the required size to replace the eardrum.
In most cases the transplant is placed under the remains of the eardrum and fixed into place.
In recent years, besides fascia, perichondrium has also been used. Perichondrium from either the penna or the tragus offer excellent material for the replacement of the eardrum: it adheres well and is congruous with its environment.
Sometimes fascia is used in the first stage of the procedure, and if that procedure was not successful, perichondrium is used in the repeated operation.
There are various ways to replace the auditory ossicles.
One of them is to prepare columellas (i.e. small columns) by carving them out of skull bone and to reconstruct the auditory ossicle system from them.
If no cholesteatoma is involved, the patient’s own auditory ossicles can be used to make columellas: especially the incus is suitable, whose long portion is often destroyed.

Besides body materials, other, artificial materials can also be used to rebuild auditory ossicles such as cement, aluminum-hydroxide, plastic, and various metals, such as platinum and gold or the combination of the two, as well as titanium.
Gold is used to replace the incus and stapes. Various kinds of tissue gluing materials are used for precise fitting.
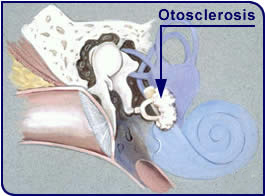
Another disease whose treatment is very successful is otosclerosis, caused by a fixation of the stapes.
This disease occurs usually bilaterally, most often in young adults, and often after childbirth. It can cause considerable psychological problems since the patient’s hearing deteriorates suddenly and fast after normal hearing up until that point in the patient’s life.

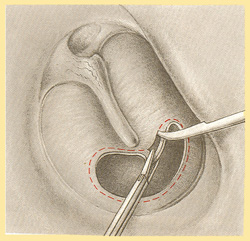
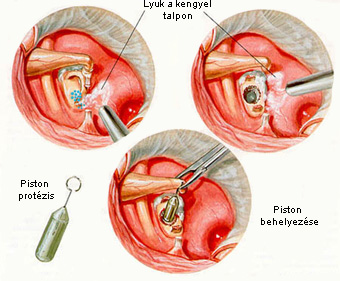
Stapedectomy
Treatment of otosclerosis is very successful with the surgical procedure called stapedectomy or stapedotomy, during which the diseased stapes is removed, its fixed base is also removed, and the prothesis is built in, connecting to the other mobile ossicles.
The prothesis is usually made out of stainless steel and tantalum (known as Schuknecht-prothesis).
The other surgical option is that the base of the stapes is not removed. In such a case a hole is made at the middle or back part of the base of the stapes, and a piston (made out of plastic or metal) is inserted into this hope, while the upper part of the piston is attached to the incus.
 The disease is relatively frequent, and the surgical rehabilitation is extremely successful.
The disease is relatively frequent, and the surgical rehabilitation is extremely successful.
Since the procedure is performed with local anthesia, patients regain their hearing already during the operation. Patients suffering from bilateral otosclerosis experience the results of the successful operation as a very positive experience.
The microsurgical restoration of various types of conductive hearing impairment has become very successful in recent years, and, as a result, today most cases of conductive hearing impairment can be surgically restored.
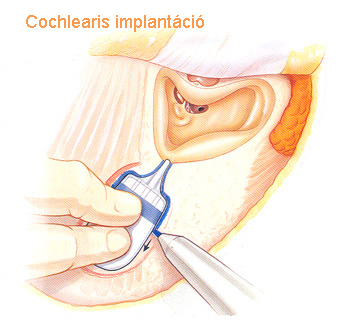
 Cochlear implantation
Cochlear implantation
In recent years completely deaf patients’ state has become possible to be surgically improved. Cochlear implants are electronic devices which turn acoustic signals into electronic signals that stimulate the auditory canal, making completely deaf patients experience sound.
It can be used with deaf patients who became deaf before the time of language acquisition (prelingual deaf) as well as those who became deaf after that period (postlingusl deaf).
 In the case of the latter group, patients soon start understanding speech, talking on the phone, and enjoying music.
In the case of the latter group, patients soon start understanding speech, talking on the phone, and enjoying music.
Cochlear implants are used with patients who can no longer hear with a hearing aid, but who also experience hearing sound after the operation. The first successful operations were performed in the late 1980s.
Since then, cochlear implants have become smaller, and the speech transforming processors they contain have been constantly discreasing in size.
The hearing improvement that can be achieved with the cochlear implants largely depends on the length of the period of the disease and hearing impairment, and on whether the patient’s hearing impairment is congenital or acquired.
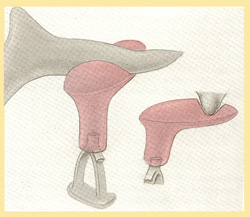
Cochlear implants consist of two parts
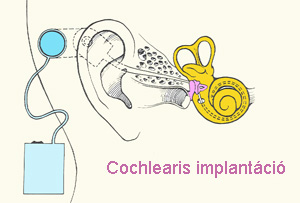 One of the parts, a platinum-iridum electrode is implanted surgically, preferably into the inner ear, while the implant itself is fixed onto the mastoid bone.
One of the parts, a platinum-iridum electrode is implanted surgically, preferably into the inner ear, while the implant itself is fixed onto the mastoid bone.
The implanted part of the device is not visible from the outside.
The other part, an external stimulating apparatus, stimulates the implant from outside.
The implantation is a microsurgical procedure requiring considerable surgical experience. The speech processor is set up about 3-4 weeks after the healing of the surgical wound.
 The pitch and frequency of the sound are set, and an audiovisual training is begun, to influence the biologically inhibited person to be open and effective again.
The pitch and frequency of the sound are set, and an audiovisual training is begun, to influence the biologically inhibited person to be open and effective again.
The rehabilitation program is complemented by auditory training and communication training as well. Among postlingual deaf patients results are very good, while among prelingual deaf patients they are better than expected.
The best results are achieved among those patients who receive the implants relatively soon after becoming deaf. Cochlear implants are a new and great opportunity for the treatment and rehabilitation of deaf patients.
The procedure offers a very good rehabilitation for most deaf patients, in some of them restoring almost full hearing, ability to talk on the phone, to listen to music, and to produce intelligible speech.
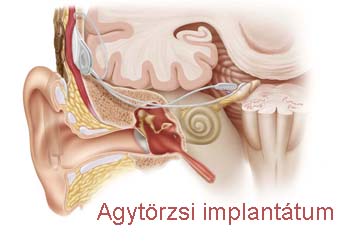 Brain stem implants
Brain stem implants
In those cases when deafness is caused by damage both to the hair cells of the inner ear and to the fibres of the auditory nerve, the restoration of hearing is possible only with the help of a brain stem implant.
In this procedure electrodes are implanted into the brain stem neurosurgically, and these can directly stimulate brain stem nuclei. Unfortunately, the results of this procedure are not as good as those of cochlear implants.
Hearing aids implanted into the middle ear
Recent years have seen attempts to implant hearing aidsinto the middle ear in case of neural hearing impairment.
These are aimed at eliminating difficulties associated with traditional hearing aids such as imperfect sound production, sound distortion, induction, and cosmetic disadvantages.
Hits: 5924




